Living with Impaired Airway Clearance?
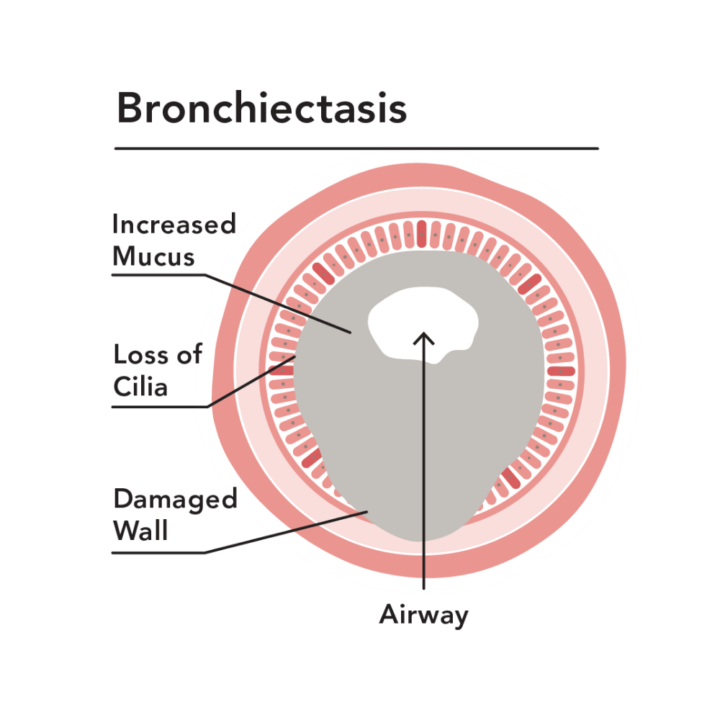
If shortness of breath, frequent cough, or chest pain is getting in the way of you enjoying life’s moments, you may be living with a chronic respiratory condition, such as COPD, cystic fibrosis, or bronchiectasis. Over your lifetime, these lung diseases can weaken the airways, making it difficult for your body to naturally clear mucus on its own so it can prevent the spread of infection.
Living with bronchiectasis has its good and bad days, or “flare ups” (a.k.a exacerbations). When this happens, you may experience a worsening of the following symptoms: