Chronic cough, shortness of breath, mucus buildup, and recurring respiratory infection are all common bronchiectasis symptoms. Although there is currently no cure for this chronic lung condition, there are ways to help manage your individual symptoms so you can breathe easier.
In this guide, you’ll find answers to common questions about bronchiectasis to help you understand its impact on your health, wellness, and life expectancy.
What Is Bronchiectasis?
Bronchiectasis (pronunciation: brong-kee-EK-tuh-sis) is a chronic lung condition that causes damage to the airways, making breathing difficult. The disease is characterized by the widening and scarring of the bronchial tubes—air passages that carry oxygen to and from the lungs.
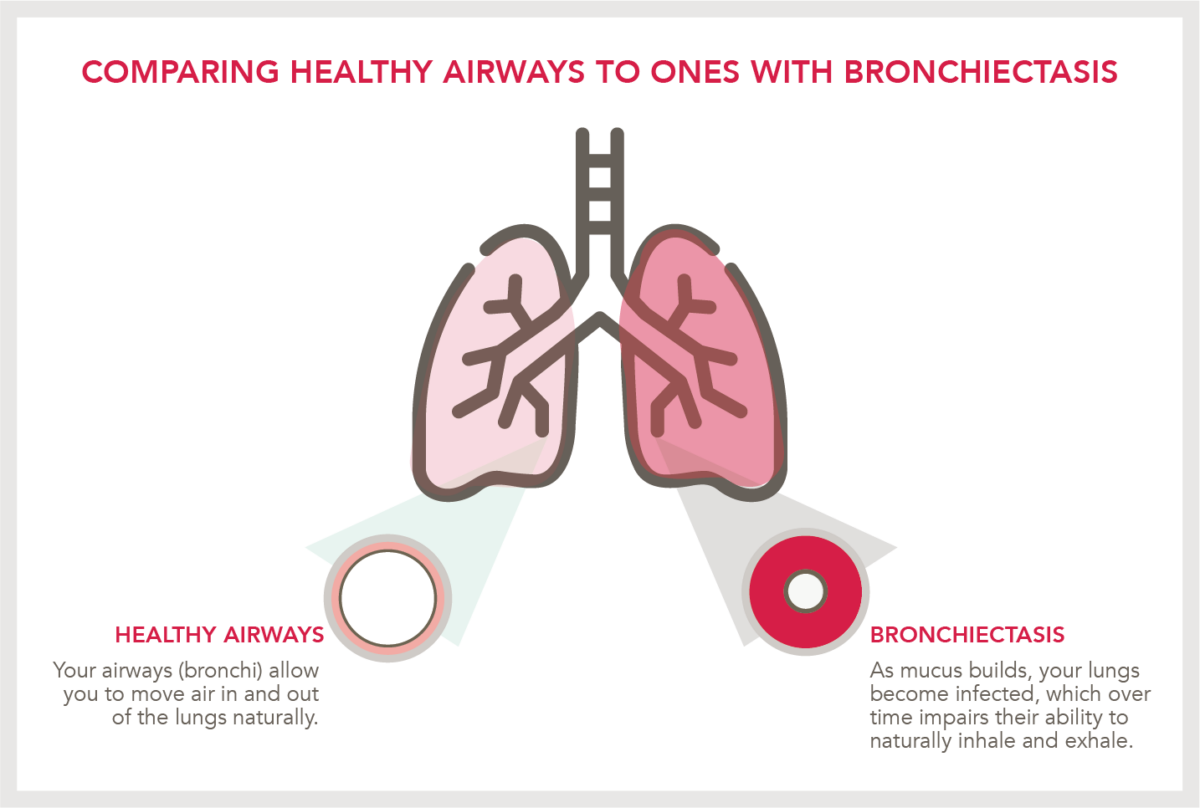
The damage can lead to a buildup of mucus and bacteria in the lungs, causing frequent infections and other serious complications.
Bronchiectasis is a progressive condition that can worsen over time if left untreated.
What Is the Most Common Cause of Bronchiectasis?
Bronchiectasis typically develops from a previous lung infection that damages the airways and leads to their widening and scarring.¹
Additionally, damage to the cilia, which are tiny-hairlike structures located along your bronchial tubes, can make it difficult for the lungs to clear mucus buildup independently. As a result, bacteria builds up and spreads throughout the lungs. This can lead to recurring infections that repeatedly damage the lungs and airways, which can then develop into bronchiectasis.²
Other factors, such as autoimmune and inflammatory diseases, Mycobacterial infections, and genetic conditions like Cystic Fibrosis, can also be the catalyst for someone developing bronchiectasis symptoms.³
Understanding Some Early Signs
Bronchiectasis symptoms can vary from person to person, but some of the most common ones include:
- Persistent cough accompanied by yellow/green sputum4
- Shortness of breath
- Chest pain
- Fatigue
- Respiratory inflammation
- Recurring lung infections
These symptoms can range from mild to severe, requiring hospitalization. If you experience any of these symptoms, seeing your clinician for an accurate diagnosis (i.e., high-resolution computerized tomography scan) and personalized treatment plan is crucial.
Does Bronchiectasis Go Away?
Unfortunately, bronchiectasis does not go away on its own. However, with proper treatment and management, you can control its symptoms and reduce the risk of complications.
What Are My Treatment Options?
Treatment options for bronchiectasis may include antibiotics to fight infections, bronchodilators to open the airways, and chest physiotherapy to help clear mucus from the lungs. In severe cases, surgery may be necessary to remove damaged lung tissue.5
Your healthcare provider will work with you to develop a personalized treatment plan based on your individual needs and bronchiectasis symptoms.
Bronchiectasis Life Expectancy
It cannot be understated that proper diagnosis and management of symptoms can help you live life to its fullest potential, even with a chronic lung condition like bronchiectasis.
Depending on various factors, such as the severity of the condition, your age and overall health, and how well the disease is managed, you can achieve a normal life expectancy. Nevertheless, repeated damage to the lungs and airways without proper treatment can be fatal.6
In addition to medical treatment, lifestyle changes, and self-care habits can help reduce the cycle of mucus buildup and infection:
- Quitting smoking is crucial, as smoking can worsen lung damage and increase the risk of infections.
- Staying hydrated and maintaining a healthy diet can also help keep mucus thin and easier to cough up.
- Regular exercise, under the guidance of a healthcare provider, can improve lung function and overall health.
- Avoiding triggers like air pollution, dust, and allergens and practicing good hygiene can also help reduce infections.
- Utilizing airway clearance techniques can also help clear mucus and other lung secretions to prevent them from accumulating and causing infections.
With proper management and care, people with bronchiectasis can lead healthy and fulfilling lives.
Managing Bronchiectasis Symptoms with HFCWO Therapy
High-frequency chest wall oscillation (HFCWO) therapy helps loosen and clear mucus from the lungs via a generator connected to a respiratory vest that you wear around the chest.
The controlled vibrations and oscillation of air help propel mucus upward, where it can easily be coughed out. HFCWO therapy is typically recommended for patients with bronchiectasis as it helps prevent mucus buildup that could lead to lung infection.
However, not all HFCWO therapy devices are the same.
The SmartVest System

The SmartVest Airway Clearance System is an inflatable vest that fits comfortably around the chest wall to deliver therapy.
Speaking of comfort, on average, SmartVest releases 91% of its air between compressions.7 This allows patients to experience more BREATHING ROOM™ during therapy vs. feeling restricted.
SmartVest delivers 360° chest wall coverage and was used in a study as part of an algorithm of care program to help patients find relief from bronchiectasis symptoms.
The results demonstrated that SmartVest helped:
- Reduce flare-ups requiring hospitalization
- Decrease antibiotic usage
- Stabilize lung function8
Bronchiectasis can be challenging to live with, but it doesn’t have to stop you from living life the way you choose. If you’re experiencing bronchiectasis symptoms, talk to your doctor about an HRCT scan to check for common signs of this condition.
If you receive a bronchiectasis diagnosis, the next step is airway clearance. You can request an informational packet to learn more about using SmartVest at home, its features, proven results, and more.
Inside each packet, we include a prescription form that you can hand to your healthcare team. We also handle the reimbursement process, so you can spend more time breathing easier and less time worrying about paperwork.
Resources
[1] National Heart, Lung, and Blood Institute. “What Is Bronchiectasis?” Retrieved from https://www.nhlbi.nih.gov/health/bronchiectasis
[2] Cleveland Clinic. “Bronchiectasis.” Retrieved from https://my.clevelandclinic.org/health/diseases/21144-bronchiectasis
[3] Cleveland Clinic. “Bronchiectasis.” Retrieved from https://my.clevelandclinic.org/health/diseases/21144-bronchiectasis
[4] American Lung Association. “Bronchiectasis Symptoms and Diagnosis.” Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/symptoms-diagnosis
[5] American Lung Association. “Treating and Managing Bronchiectasis.” Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/treating-and-managing
[6] National Health Service (NHS). “Overview: Bronchiectasis.” Retrieved from https://www.nhs.uk/conditions/bronchiectasis/
[7] Pokorney J. Comparison of Oscillatory Trough Pressure Generated by High Frequency Chest Wall Oscillation (HFCWO) Systems: A White Paper.
[8] Powner J, Nesmith A, Kirkpatrick DP, Nichols JK, Bermingham B, Solomon GM. Employment of an algorithm of care including chest physiotherapy results in reduced hospitalizations and stability of lung function in bronchiectasis. BMC Pulm Med. 2019;19(1):82. Published 2019 Apr 25