Abstract
Introduction: The goals of bronchiectasis treatment are to mobilize airway secretions to reduce pulmonary infections, minimize the number of respiratory exacerbations, enhance ventilation, and improve a person’s quality of life. High frequency chest wall oscillation (HFCWO) is widely used for improving airway clearance in patients with a range of diseases and conditions that clinically benefit from increased bronchial drainage. However, only a limited number of studies have evaluated the use of HFCWO in patients with non-cystic fibrosis bronchiectasis. This case review study was designed to assess the clinical outcomes of the SmartVest® Airway Clearance System (Electromed, Inc, New Prague, MN, USA) on exacerbation-related healthcare utilization and medication in subjects with non-cystic fibrosis bronchiectasis.
Methods
Subjects (N=59) with confirmed diagnosis of non-cystic fibrosis bronchiectasis, who had been using SmartVest for at least one year, and whose medical records were available for one year prior to initiation of SmartVest therapy were included. Subjects were also contacted and interviewed by phone to collect information regarding exacerbation-related healthcare utilization and medication needs during the first year after the start of SmartVest therapy. The frequency of hospitalizations, total number of hospital and emergency room (ER) visits, and antibiotic and steroid use for one year before and after initiation of SmartVest therapy were determined. Compliance to treatment, as prescribed by the subject’s physician, was also determined. To provide statistical evidence that SmartVest therapy significantly decreased these frequencies, a paired t-test was used.
Results
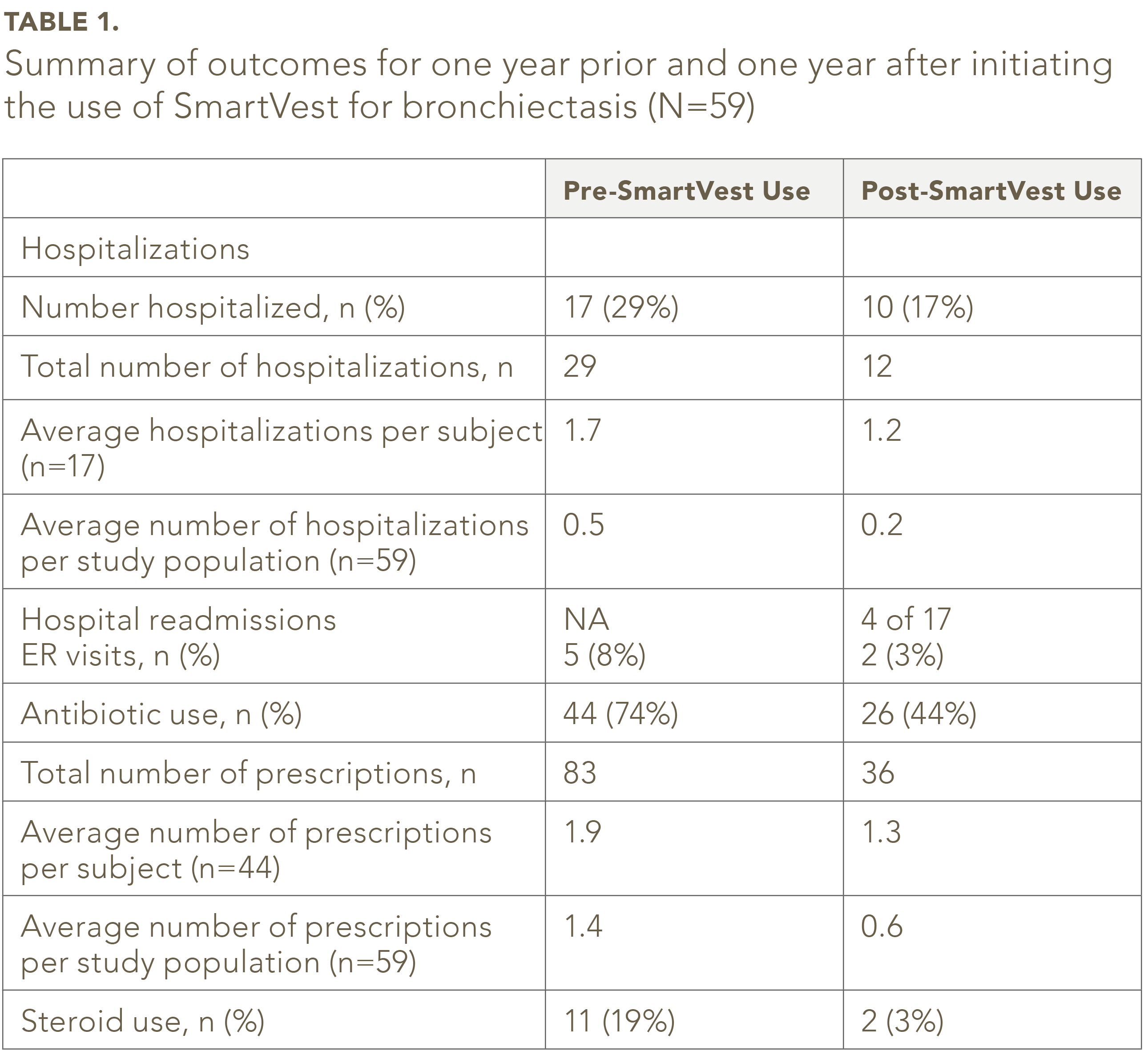
The number of subjects hospitalized for a bronchiectasis related exacerbation was approximately 1.5 fold lower (P=0.007) after using the SmartVest for one year (10 of 59 or 17%) compared to the year before SmartVest use (17 of 59 or 29%). In addition, 11 of the 17 subjects (65%) who reported a hospital admission prior to SmartVest use did not require a hospital readmission for an exacerbation after SmartVest use. The number of ER visits decreased 63% (from 8% to 3%, p=0.083) with the use of SmartVest. The percentage of subjects using antibiotics decreased from 74% in the year prior to SmartVest therapy to 44% in the year following initiation of therapy (P=0.0000047). The number of antibiotic prescriptions per subject declined with SmartVest use (from 1.9 to 1.3 per subject) as well as the prescriptions per the entire study population (from 1.4 to 0.6 per population). SmartVest therapy was also associated with a greater than six fold decrease (19% vs. 3%) in steroid use (P=0.0020). Although not included in the phone interview call protocol, 40 of the 59 subjects (68%) interviewed reported a significant improvement in their quality of life.
Conclusion
This outcomes-based case review of SmartVest use demonstrated a statistically significant reduction in bronchiectasis-related healthcare utilization and antibiotic and steroid use. The results validate and are consistent with the SmartVest’s clinical utility of improving pulmonary mucus clearance and bronchial drainage and decreasing respiratory related exacerbations in non-cystic fibrosis bronchiectasis patients.
Introduction
Bronchiectasis is defined as an irreversible dilation and destruction of the bronchi with significantly reduced clearance of pulmonary secretions.1,2 The disease is associated with recurrent lower respiratory infections, inflammation, reduction in pulmonary function, impaired respiratory secretion clearance, increased hospitalizations and medication use, and increased morbidity and mortality.3-5 The overall prevalence of non- cystic fibrosis bronchiectasis is about 52 per 100,000 adults and the mean age at diagnosis is 61 years.6 The incidence of hospitalization due to non-cystic fibrosis bronchiectasis is rising and is markedly increased for patients 50 years of age or older.5,6 Bronchiectasis patients annually averaged: 6 more outpatient encounters, 27 more days of antibiotic treatments, and 2 more days in the hospital.6,7 In 2005, the estimated cost for non-cystic fibrosis bronchiectasis was $630 million annually in the United States.6,7
The goals of bronchiectasis treatment are to mobilize airway secretions to reduce respiratory infections, minimize the number of exacerbations, enhance ventilation, and improve a person’s quality of life.8,9 Patients with non-cystic fibrosis bronchiectasis can have difficulty clearing airway secretions, and can benefit from airway clearance therapy.6 Efficient removal of retained respiratory secretions, in addition to the use of antibiotics and other medications can lessen episodes of acute illness and slow the rate of progressive deterioration.6,10 A number of therapeutic methods are currently used to clear airway secretions in patients with pulmonary disease, respiratory mucus impairment, or who are at risk of developing either one of those conditions.8 These methods generally aim to promote secretion clearance by reducing mucus viscosity and using shear forces to release the mucus from the lung wall.
High frequency chest wall oscillation (HFCWO) is used for airway clearance in patients with a range of diseases and conditions, including genetic and immunological disorders, neuromuscular diseases, and obstructive pulmonary conditions such as asthma and chronic obstructive pulmonary disease (COPD).11-14 A number of clinical studies have demonstrated the safety and efficacy of HFCWO, primarily in patients with cystic fibrosis.6,11,15-17 Typically, HFCWO delivers compression pulses to the chest wall through an inflatable vest (or wrap) connected to an air pulse generator.6 The generator produces an alternating flow of air into the vest that rapidly compresses and releases the chest wall at a variety of selectable frequencies and pressures, resulting in an oscillation in airflow within the airways that act to loosen, thin, and propel mucus toward the major airways where it can be expectorated or suctioned away.18,19 During HFCWO, all segments of the lungs are treated simultaneously.6 HFCWO can lead to changes in lung volume of 15 to 57 mL and in flow up to 1.6 L/s, which generate effective coughing to mobilize secretions.20 The therapy requires minimal activity from the user and is technique independent.6 Although HFCWO is well tolerated and has shown efficacy in improving mucociliary clearance in patients with cystic fibrosis, there is currently very little evidence of usage or benefit in adults with non-cystic fibrosis bronchiectasis.20 Knowing the clinical utility and efficacy of a given device are of considerable clinical importance and also impacts patient accesses to this technology. Clinical efficacy is one of the considerations used by Medicare, Medicaid, and private insurers to make coverage and reimbursement decisions. The objective of this outcomes-based case review study was to determine whether that SmartVest Airway Clearance System (Electromed, Inc., New Prague, MN, USA) was associated with a reduction in exacerbation-related healthcare utilization and medication use in patients with non-cystic fibrosis bronchiectasis.
Methods
The study was performed in accordance with the declaration of Helsinki. The Western Institutional Review Board waved the necessity of the protocol being reviewed by an Institutional Review Board, and the requirement for obtaining written informed consent from subjects, as all subjects had signed a HIPAA privacy agreement prior to the release of their medical records to the study’s sponsor.
Study Subjects
Patients with a diagnosis of non-cystic fibrosis bronchiectasis, who had been using SmartVest for at least one year, and whose medical records were available for one year prior to initiation of SmartVest therapy were eligible for study recruitment. Subjects, who had not been compliant with SmartVest therapy as prescribed by their physician, had died, or who were unable to be contacted by phone were excluded from the study. Compliance was determined by patient follow-up via phone interview, returned compliance report or recorded clock hours in the generator.
Study Design
The Electromed patient database, which includes patient medical records, was screened for potential subjects who met the inclusion/exclusion criteria. Patient medical records were reviewed for all bronchiectasis-related exacerbations that occurred within one year of starting SmartVest therapy, and the number hospitalizations, ER visits, and antibiotic and/or steroid use exclusively related to the subject’s existing respiratory condition were also recorded. All prior use of any alternative airway clearance devices prior to using the SmartVest was also recorded. Subjects were contacted and interviewed by phone to collect the same information for the one year following initiation of SmartVest therapy. All phone interviews were performed by the same licensed respiratory therapist (C Beaner).
The questionnaire was developed by Electromed for the exclusive purpose of this study. During the phone interview, the subject was asked the following questions:
- Are you still using the SmartVest according to your Doctor’s prescription? If no, when did you stop using it?
- Since you began using the SmartVest, have you required treatment with antibiotics or prednisone to treat a respiratory infection?
- Since you began using the SmartVest, have you required hospitalization related to your respiratory condition? If yes, where?
- Since you began using the SmartVest, have you required a visit to the emergency room related to your respiratory condition? If yes, where?
All data was summarized descriptively. To provide evidence that SmartVest therapy significantly decreased these frequencies, a paired t-test was used.
Results
Of the 104 bronchiectasis subjects identified from the Patient Database who met the inclusion/exclusion criteria, two were found to be deceased per data base review. Of the remaining 102 subjects, all received a phone call attempt. Fifty-nine subjects met the inclusion/exclusion criteria required to be included in the study. The other 43 subjects were not included in the study for several reasons: eight were not able to be contacted due to incorrect contact information, 2 were reported to be deceased by the caregiver, 1 subject was incoherent, 25 subjects did
not respond to calls and/or multiple voicemail messages, and seven subjects were found to be noncompliant with SmartVest treatment as prescribed by their physician.
SmartVest treatment was associated with reduced bronchiectasis-related healthcare utilization (Table 1). The number of subjects hospitalized for a bronchiectasis related exacerbation was approximately 1.5 fold higher (P=0.007) during the year prior to SmartVest use (17 of 59 or 29%) compared to one year after its use (10 of 59 or 17%). Of those hospitalized, 11 of 17 subjects (65%) who reported an admission prior to SmartVest use did not require a readmission for an exacerbation after one year of SmartVest use. The number of ER visits decreased from 8% to 3% (63% decrease) with the use of the SmartVest. The subjects that had ER visits prior to SmartVest use of were not the same subjects who visited the ER after starting therapy.
The use of SmartVest was associated with a statistically significant decrease in the use of antibiotics and steroids for treating a bronchiectasis related exacerbation (P=0.000004
and P=0.002 respectively). The percentage of subjects using antibiotics decreased from 74% prior to SmartVest use to 44% after one year of SmartVest therapy. The number of prescriptions also decreased per subject who used an antibiotic (from 1.9 to 1.3 per subject) as well as the prescriptions per the entire study population (from 1.4 to 0.6 per population). SmartVest therapy was also associated with a greater than six fold decrease (19% vs. 3%) in steroid use (P=0.0020). Although not included in the phone interview protocol, 40 of the 59 subjects (68%) interviewed unreservedly reported a significant improvement in their quality of life.
Discussion
Non-cystic fibrosis bronchiectasis is a serious progressive condition related to permanent and abnormal widening of the airways which may require extensive medical care including medications and hospitalizations. Currently, there is limited information regarding the efficacy of treating non-cystic fibrosis bronchiectasis with HFCWO, and no prior study has evaluated the use of SmartVest in this patient population. This case review outcome study was designed to gain insight into the efficacy of the SmartVest system in treating non-cystic fibrosis bronchiectasis by evaluating changes in bronchiectasis-related healthcare utilization and medication use due to a related exacerbation following one year of SmartVest treatment. We found that SmartVest was associated with a significant reduction in hospitalizations both per patient and per study population. It also resulted in a significant reduction of associated medication use, including a reduced number of antibiotic prescriptions and steroid use both per subject and per study population.
Our findings are consistent with SmartVest’s clinical utility of improving airway clearance and bronchial drainage in patients with a range of diseases and conditions. The improvement in airway clearance and sputum production is reported by a prior study that evaluated SmartVest in the treatment of subjects with moderate chronic obstructive pulmonary disease (COPD) (N=22).21 Subjects received four weeks of SmartVest therapy. Use of SmartVest was associated with a decline in sputum production, although this did not reach statistical significance compared with conventional treatment; the mean change in sputum volume was −2.6 mL (range −53 to +27 mL) for SmartVest, and +6 mL (range −70 to +40 mL) for conventional treatment (P=0.06). The degree of sputum volume decrease was related to baseline sputum production (P=0.02). The HFCWO modality delivered by the SmartVest system was well tolerated in patients who often had significant disability including shortness of breath at rest. No subjects dropped out due to intolerance of the device.
Chakravorty, et. al., (2011) also found that there was clinically improvement in patient reported quality of life with SmartVest therapy. Subjects reported improvement in the five-symptom score (rating of cough, sputum, wheeze, shortness of breath, and exercise tolerance) (P=0.02).21 SmartVest therapy significantly improved the symptom dimension of the St. George’s Respiratory Questionnaire (SGRQ) (P=0.02), an instrument that evaluates health-related quality of life.21 In contrast, there was no change in the self-reported symptom or SGRQ scores in patients who received conventional treatment.21 Although, we did not prospectively plan to collect quality of life information during our study, 68% of the subjects during the phone interview commented that the use of SmartVest had appreciably improved their quality of life.
Medicare, Medicaid and other insurance policies for coverage and reimbursement of HFCWO therapies tend to be similar. Medicare will cover HFCWO for bronchiectasis if the patient has a confirmed diagnosis, has a history of more than two exacerbations per year requiring antibiotics or documentation of a daily productive cough for at least 6 continuous months, and well-documented failure of standard treatment devices (eg, positive expiratory pressure (PEP)) to adequately mobilize secretions. The efficacy in airway clearance demonstrated by HFCWO in different populations, use of SmartVest in patients with COPD, and now by this bronchiectasis outcomes-based study supports the argument for insurance coverage by payers. Importantly, the use of SmartVest significantly decreased the number of hospitalizations and antibiotic/steroid use in this study. The reduction of hospitalizations, including readmissions, would be expected to significantly impact healthcare costs, as the cost of inpatient care is high; a study performed in 2009 found that median cost of inpatient care from 1993 to 2006 for non-cystic fibrosis bronchiectasis was $7,837 (USD).5 The same study found that the annual age-adjusted hospitalizations rate was 16.5 hospitalizations per 100,000 population.5 This is particularly important in older patients as the rate of hospitalization markedly increases above the age of 50 years, and particularly in older women.5 A 2005 study found that patients with non-cystic fibrosis bronchiectasis averaged 2.0 additional days in the hospital, had 6.1 additional outpatient encounters, 27.2 more days of antibiotic therapy, and total excess medical expenditure of $5681 (USD).6,7
In conclusion, this study found that SmartVest significantly reduced bronchiectasis-related healthcare utilization and antibiotic and steroid use which is consistent with SmartVest’s clinical utility of improving airway clearance and bronchial drainage. Larger studies are planned to further evaluate the efficacy and cost-benefit of SmartVest in treating bronchiectasis patients.
References
- Barker AF. Bronchiectasis. N Engl J Med. 2002;346(18):1383-1393. 10.1056/NEJMra012519
- Habesoglu MA, Ugurlu AO, Eyuboglu FO. Clinical, radiologic, and functional evaluation of 304 patients with bronchiectasis. Ann Thorac Med. 2011;6(3):131-136. 10.4103/1817-1737.82443
- King PT, Holdsworth SR, Freezer NJ, Villanueva E, Gallagher M, Holmes PW. Outcome in adult bronchiectasis. COPD. 2005;2(1):27-34.
- Alzeer AH, Masood M, Basha SJ, Shaik SA. Survival of bronchiectatic patients with respiratory failure in ICU. BMC Pulm Med. 2007;7:17. 10.1186/1471-2466-7-17
- Seitz AE, Olivier KN, Steiner CA, Montes de Oca R, Holland SM, Prevots DR. Trends and burden of bronchiectasis-associated hospitalizations in the United States, 1993-2006. Chest. 2010;138(4):944-949. 10.1378/chest.10-0099
- Braverman J, Miller H. High-frequency chest compression: a practical therapy for patients with bronchiectasis. Respiratory Therapy. 2008;3(1):22-26.
- Weycker D, Edelsberg J, Oster G, Tino G. Prevalence and economic burden of bronchiectasis. Clinical Pulmonary Medicine. 2005;12:205-209.
- Fibrosis. AoCPiC. Standards of care and good clinical practice for the physiotherapy management of cystic fibrosis 2011 [cited 2016 January 4]. Available from: https://www. cysticfibrosis.org.uk/media/82076/CD_Standards_of_Care_ Physio_Jun_11.pdf.
- O’Donnell AE. Bronchiectasis. Chest. 2008;134(4):815-823. 10.1378/chest.08-0776 10. McShane PJ, Naureckas ET, Tino G, Strek ME. Non- cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2013;188(6):647-656.
- 1164/rccm.201303-0411CI
- Arens R, Gozal D, Omlin KJ, et al. Comparison of high frequency chest compression and conventional chest physiotherapy in hospitalized patients with cystic fibrosis. Am J Respir Crit Care Med. 1994;150(4):1154-1157. 10.1164/ajrccm.150.4.7921452
- Fink JB, Mahlmeister MJ. High-frequency oscillation of the airway and chest wall. Respir Care. 2002;47(7):797-807.
- Hansen LG, Warwick WJ. High-frequency chest compression system to aid in clearance of mucus from the lung. Biomed Instrum Technol. 1990;24(4):289-294.
- Lange DJ, Lechtzin N, Davey C, et al. High-frequency chest wall oscillation in ALS: an exploratory randomized, controlled trial. Neurology. 2006;67(6):991-997. 10.1212/01. wnl.0000237439.78935.46
- Warwick WJ, Hansen LG. The long-term effect of high-frequency chest compression therapy on pulmonary complications of cystic fibrosis. Pediatr Pulmonol.
1991;11(3):265-271. - Kluft J, Beker L, Castagnino M, Gaiser J, Chaney H, Fink RJ. A comparison of bronchial drainage treatments in cystic fibrosis. Pediatr Pulmonol. 1996;22(4):271-274. 10.1002/
(SICI)1099-0496(199610)22:4<271::AID-PPUL7>3.0.CO;2-P - Scherer TA, Barandun J, Martinez E, Wanner A, Rubin
EM. Effect of high-frequency oral airway and chest wall oscillation and conventional chest physical therapy on expectoration in patients with stable cystic fibrosis. Chest. 1998;113(4):1019-1027. - Osman LP, Roughton M, Hodson ME, Pryor JA. Short-term comparative study of high frequency chest wall oscillation and European airway clearance techniques in patients
with cystic fibrosis. Thorax. 2010;65(3):196-200. 10.1136/thx.2008.111492. - Chatburn RL. High-frequency assisted airway clearance. Respir Care. 2007;52(9):1224-1235; discussion 1235-1227.
- Nicolini A, Cardini F, Landucci N, Lanata S, Ferrari-Bravo M, Barlascini C. Effectiveness of treatment with high-frequency chest wall oscillation in patients with bronchiectasis. BMC Pulm Med. 2013;13:21. 10.1186/1471-2466-13-21
- Chakravorty I, Chahal K, Austin G. A pilot study of the impact of high-frequency chest wall oscillation in chronic obstructive pulmonary disease patients with mucus hypersecretion. Int J Chron Obstruct Pulmon Dis. 2011;6:693-699. 10.2147/COPD. S22896